Chiropractic SOAP notes are a standardized framework for keeping track of a patient’s progress during treatment.
If you’re like a lot of chiropractors, you might be in the habit of leaving your notes to complete the next day. The problem is that they can quickly pile up and leave you feeling behind.
Wouldn’t it be nice to leave the day with completed SOAP notes?
This blog post will cover everything you should include in your chiropractic SOAP notes and how to write them faster so you never have to get behind.
What Are SOAP Notes and Why Are They Important for Chiropractic Practices?
SOAP notes are a method of documentation in the healthcare industry used to record a patient’s chief complaint and treatment plan. They provide a record of a patient’s progress over time.
SOAP notes are also necessary for insurance purposes. Additionally, they keep you compliant and protect you against insurance audits and fines due to CPT coding procedure violations or even a malpractice suit.
SOAP (which stands for Subjective, Objective, Assessment and Plan) provides a structured framework for approaching these notes. This is a universal format, which means that the notes can be shared with other healthcare providers. This way, information is always easily accessible.
What Do You Write in a SOAP Note? The Four Main Sections
Now we’ll go into detail about what each section of chiropractic SOAP notes should include:
Subjective
The subjective portion of the SOAP note outlines the patient’s chief complaint as stated by the patient, which is why it’s referred to as the subjective portion of the SOAP note. For chiropractors, this likely looks like back pain, neck pain or another neuromuscular issue.
One key point to keep in mind is that if a patient has both a sore neck and a sore back, it’s important to record subjective information for both of these complaints.
Other information to include in this section includes:
- Cause
- Specific date of onset
- Type of pain (i.e. throbbing or dull)
- If the pain is constant or intermittent
- Severity of pain (on a pain scale)
- Activities that improve and worsen pain
- Any unrelated symptoms
- Pain level since last visit (worse/improved)
The first SOAP note will always have a more lengthy subjective position than future chiropractic SOAP notes as the first SOAP note always contains the entire history of the patient. Future notes, though, can simply outline any changes in symptoms or even the current level of pain.
Fun Fact: With Yocale’s chiropractic practice management software, you can have clients complete the subjective portion of the SOAP note before they come in, ultimately cutting down your SOAP note time. Other types of Yocale’s software, such as med spa practice management software or mental health scheduling software have the same features.
(You can also have clients complete the subjective portion of the SOAP note when they arrive to the office via a tablet. You’ll be able to hide the Objective/Assessment/Plan sections of the note and lock access to everything except for the SOAP note).
Have patients complete the subjective portion of SOAP notes
Objective
The objective portion of the SOAP note covers measurable data. Tenderness and muscle spasm are the standards here as well as testing for range of motion. This section may even include various tests, such as neurological or orthopedic tests.
This section doesn’t change until after you’ve done your reexamination, which typically won’t happen until three or four more weeks after the patient’s first visit.
It is generally this section of the SOAP note that requires the most amount of time.
Assessment
This section outlines the patient’s diagnosis based on the information above – that is, the subjective information from the client as well as the examinations obtained during the objective portion of the SOAP note.
It will also include the patient’s prognosis.
With subsequent chiropractic SOAP notes, this section will remain the same (and you can say as such) unless the client has developed a new injury.
Plan
This section outlines the treatment plan for what you’d like to do in the future in order to address the client’s condition. It includes therapeutic treatment, as well as the duration and frequency, and might include lab work or exercise/lifestyle modifications to name a few.
Just like the Objective and Assessment sections, the Plan will also stay the same after the first note until reexamination in three or four weeks.
You must also record what treatments you used, such as therapeutic ultrasound or TENS application.
A Chiropractic SOAP Note Template
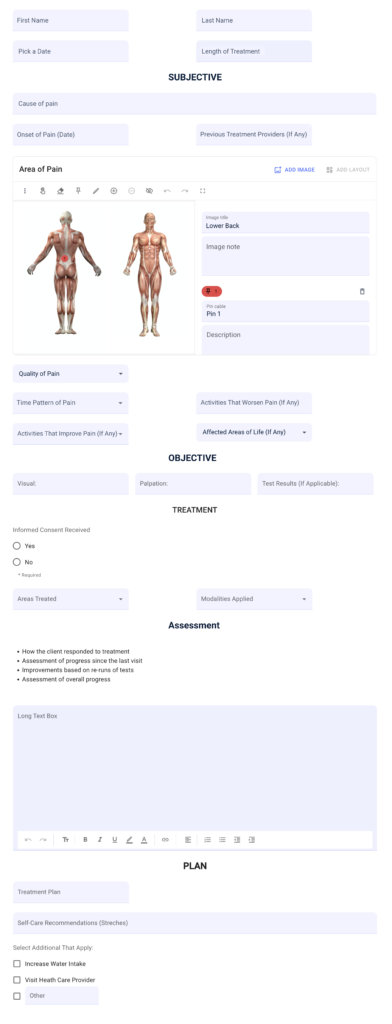
Have patients complete the subjective portion of SOAP notes
How Long Should a SOAP Note Be? The Importance of Thorough SOAP Notes
A common question is “How long should a SOAP note be”? Chiropractic SOAP notes are typically a page in length, but most of this information is simply checking off various boxes and not necessarily a lot of writing. In fact, SOAP notes don’t need to take more than five minutes to complete.
At the end of the day, thorough chiropractic SOAP notes will ensure that you’re able to assess the results of your treatment, and they’ll protect you in the event that you’re ever sued.
In the event that you’re audited, they’ll prove that you followed the proper procedures and billed patients correctly.
Are Your SOAP Notes Thorough?
A good way to assess whether your chiropractic SOAP notes are thorough enough is to ask yourself if another chiropractor could realistically continue treatment if you were to stop practicing tomorrow.
If the answer is yes, your notes should be thorough enough.
How to Write Faster Chiropractic SOAP Notes
1. Have Clients Complete the Subjective Portion of Your SOAP Notes
You can use chiropractic management software like Yocale to have clients complete the subjective portion of your SOAP notes with you during their visit or in advance of appointments via practice management software.
When clients book appointments online, they’ll be automatically sent a copy of your SOAP notes. You can even hide every aspect of the note except for the Subjective portion.
2. Complete SOAP Notes During Treatment
Another way of writing faster SOAP notes (or at least avoiding having them become a chore) is to simply write your notes during your treatments. A great way to do this is by using cloud-based practice management software. This way, your chiropractic SOAP notes will be accessible from wherever you are.
3. Use Voice Dictation
Another way to reduce time spent on your SOAP notes is to use voice dictation. This is all made possible by chiropractic practice management software.
4. Use Chiropractic Practice Management Software
If it wasn’t obvious yet, chiropractic practice management software is key to reducing SOAP note time.
Not only can practice management software like Yocale help with all of the above, but you can also insert favorite text, such as “Same as last treatment,” with the click of a button, thereby cutting down unnecessary time even more.
Write faster, more compliant SOAP notes
Wrapping it Up
Chiropractic SOAP notes are critical to providing a record of a patient’s progress over time; not only is this important for treatment purposes, but it’s also important for insurance purposes and keeping you compliant.
While many chiropractors tend to get behind on their SOAP notes, the good news is that chiropractic practice management software can really help make the process much easier so they don’t become a chore.
Other Blog Posts You Might Be Interested in Reading:
Interested in learning more about chiropractic practice management software? Book a demo with a Yocale product specialist today.